Childhood Cancer pediatric brain tumors

Childhood Cancer Pediatric Brain Tumors
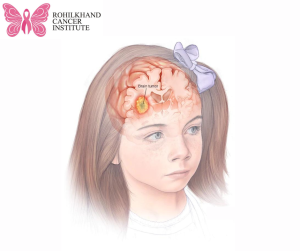
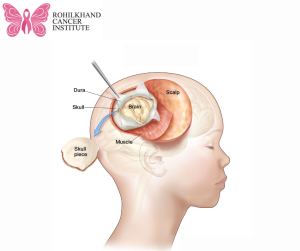
Cell growths that begin in or close to the brain in children are known as Childhood Cancer Pediatric Brain tumour growths have the potential to enlarge and exert pressure on adjacent brain regions. Headaches and nausea are two symptoms that may result from this.
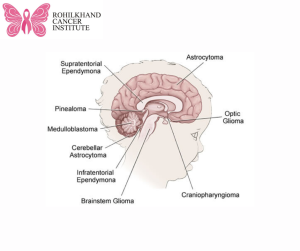
There are numerous kinds of brain tumours in children. While some grow slowly, others grow swiftly. Not all of them are malignant; some are. Brain tumours are another name for noncancerous brain tumours.
There are numerous kinds of brain tumours in children. While some grow slowly, others grow swiftly. Not all of them are malignant; some are. Brain tumours are another name for noncancerous brain tumours.
The most effective course of treatment for a child’s brain tumour depends on its type. The location of the tumour, whether it has migrated outside of the brain, your kid’s age, and general health are among factors that the medical team treating your child takes into account.
The course of treatment for brain tumours in children and adults is frequently very varied. Seek treatment in a hospital that has experience treating kids with brain tumours because of this.
Symptoms
Depending on where the tumour is located in the brain, the symptoms of a paediatric brain tumour can change. The tumor’s size and rate of growth may also have an impact on symptoms.
When a child has a brain tumour, some of the more typical symptoms and indicators are
(1) Nausea and vomiting.
(2) Headaches, which could increase in frequency and intensity. When a youngster remains silent, a parent may observe that the child is angrier than normal.
(3) alterations in eyesight, like double vision. When a youngster tries to gaze at something, they may squint or conceal one eye, which is something parents may notice in silent children.
Additional indications and manifestations could be:
(1) Slurred speech.
(2) Trouble walking.
(3) Hearing problems.
(4) Memory problems.
(5) Trouble swallowing.
(6) Difficulty with balance.
(7) Confusion and irritability.
(8) Personality or behavior changes.
(9) Changes in the way the eyes move.
(10) A fuller soft spot on the skull in babies.
(11) Weakness or drooping on one side on the face.
(12) Weakness or loss of sensation in an arm or a leg.
(13) Seizures, especially in a child who hasn’t had a seizure before.
When to visit a physician
If your child’s symptoms are concerning you, schedule a visit with their physician or another medical expert.
Causes
A paediatric brain tumor’s aetiology is typically unknown.
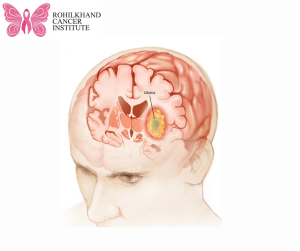
Brain cells undergo genetic alterations that lead to the development of paediatric brain tumours. The instructions that inform a cell what to do are encoded in its DNA. The DNA in healthy cells contains instructions on how to divide and expand at a specific rate. The cells are instructed to die at a predetermined time. Different instructions are given by the altered DNA in tumour cells. The alterations instruct the tumour cells to proliferate rapidly. When healthy cells would die, tumour cells can survive. There are too many cells as a result.
The excess cells may aggregate into a lump known as a tumour. Growing tumours may put pressure on adjacent brain tissue. Swelling and other changes in the surrounding brain tissue can occasionally be caused by a developing tumour.
Some tumour cells undergo further DNA alterations that cause them to become cancerous cells. Healthy tissue can be invaded and destroyed by cancer cells. Cancer cells can occasionally separate and travel outside of the brain. The fluid that surrounds the brain and spinal cord is often where brain cancer spreads. Cerebrospinal fluid is the term for this fluid.
Factors at risk
The following variables could raise a child’s risk of brain tumours:
Younger age
Tumours of the brain can occur at any age. Brain tumours in children typically affect individuals under the age of five more frequently.
Exposure to radiation
Brain tumours are more common in children after head radiation therapy treatments. For instance, receiving radiation treatment for one kind of brain tumour may make it more likely that you will get another kind.
Weakened immune system
Paediatric brain tumour risk may increase if the body’s immune system, which fights germs, is compromised by medication or disease. Children undergoing immunosuppressive medication, such as those recovering from organ transplants, are considered to have compromised immune systems. HIV infection is one medical disease that might compromise immunological function.
Genetic syndromes that run in families
Children who have certain genetic abnormalities that run in families may be more susceptible to brain tumours. As examples, consider:
(1) Gorlin syndrome.
(2) Turcot syndrome.
(3) Tuberous sclerosis.
(4) Neurofibromatosis 1.
(5) Neurofibromatosis 2.
DNA testing on your child can determine whether or not they have these syndromes.
Prevention
Brain tumours in children cannot be prevented. You did not do anything to cause your child’s brain tumour, if it occurs.