Thyroid cancer

Thyroid cancer
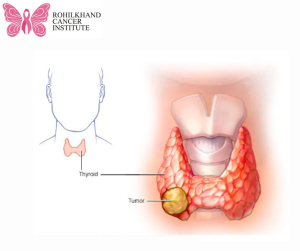
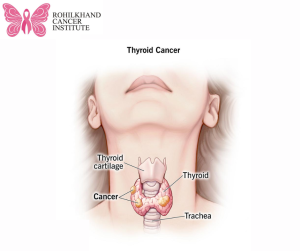
Cells begin to proliferate in the thyroid and eventually become thyroid cancer. The thyroid is a butterfly-shaped gland that sits immediately below the Adam’s apple at the base of the neck. Hormones that control blood pressure, body temperature, heart rate, and weight are produced by the thyroid.
At initially, thyroid cancer may not show any signs. However, when it gets bigger, it might produce symptoms and indicators such neck swelling, voice changes, and swallowing difficulties.
There are various forms of thyroid cancer. The majority of varieties grow slowly, while some can be extremely aggressive. With treatment, most thyroid cancers are curable.
There appears to be a rise in thyroid cancer cases. Improved imaging technology may be the reason for the increase, as it enables medical professionals to detect tiny thyroid malignancies on CT and MRI scans performed for other purposes (incidental thyroid cancers). When thyroid tumours are discovered in this manner, they are typically tiny tumours that react well to therapy.
Symptoms
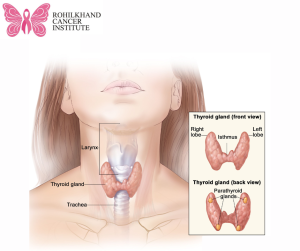
The majority of thyroid tumours don’t exhibit any early warning signs or symptoms. As thyroid cancer spreads, it could result in:
(1) Difficulty swallowing
(2) Pain in your neck and throat
(3) Swollen lymph nodes in your neck
(4) Changes to your voice, including increasing hoarseness
(5) A feeling that close-fitting shirt collars are becoming too tight
(6) A lump (nodule) that can be felt through the skin on your neck
When to visit a physician
Make an appointment with your healthcare physician if you encounter any symptoms or indicators that concern you.
Causes
When DNA alterations occur in thyroid cells, thyroid cancer results. The instructions that inform a cell what to do are encoded in its DNA. The alterations, known to scientists as mutations, instruct the cells to proliferate and expand quickly. When healthy cells would naturally perish, the cells continue to exist. A tumour is a mass formed by the cells that are collecting.
The tumour has the potential to develop, infiltrate surrounding tissue, and travel (metastasise) to the neck lymph nodes. Occasionally, cancer cells have the ability to travel to other areas of the body, including the lungs, bones, and neck.
It is unknown what causes the DNA alterations that lead to thyroid cancer in the majority of cases.
Thyroid cancer types
Based on the sorts of cells discovered within the tumour, thyroid cancer is categorised into different forms. When a sample of tissue from your cancer is studied under a microscope, your type is found. Treatment options and prognosis are based on the type of thyroid cancer.
Thyroid cancer comes in various forms.
Differentiated thyroid cancers.This wide category encompasses thyroid cancers that originate in the cells responsible for producing and storing thyroid hormones. Follicle cells are the name given to these cells. When examined under a microscope, differentiated thyroid cancer cells resemble normal cells.
Papillary thyroid cancer. The most prevalent kind of thyroid cancer is this one. Though it can occur at any age, persons between the ages of 30 and 50 are the most commonly affected. Even in cases when the cancer cells spread to the neck lymph nodes, the majority of papillary thyroid tumours are tiny and respond effectively to treatment. A tiny percentage of papillary thyroid cancers are aggressive, and they have the potential to travel to other parts of the body or enlarge to damage neck tissues.
Follicular thyroid cancer. Those older than 50 are typically affected by this uncommon kind of thyroid cancer. It is rare for follicular thyroid cancer cells to migrate to the neck lymph nodes. However, some large, aggressive tumours have the potential to spread to other body areas. Most frequently, follicular thyroid cancer spreads to the bones and lungs.
Hurthle cell thyroid cancer. There originally existed a belief that this uncommon kind of thyroid cancer belonged to the follicular subtype. Because the cancer cells behave differently and react to therapies differently, it is now regarded as a distinct kind. Aggressive Hurthle cell thyroid tumours can grow to affect neck tissues and spread to other parts of the body.
Poorly differentiated thyroid cancer. Compared to other differentiated thyroid tumours, this uncommon kind of thyroid cancer is more aggressive and frequently does not respond to standard treatments.
Anaplastic thyroid cancer. Thyroid cancer of this uncommon kind spreads swiftly and might be challenging to cure. Treatments, however, may be able to halt the disease’s advancement. People older than 60 are more likely to develop anaplastic thyroid cancer. Severe symptoms and indicators may include rapidly worsening neck swelling, which can make breathing and swallowing difficult.
Medullary thyroid cancer. The C cells of the thyroid, which generate the hormone calcitonin, are the first to develop in this uncommon form of thyroid cancer. At a very early stage, elevated blood levels of calcitonin can be a sign of medullary thyroid cancer. A gene called RET that is inherited from parents to offspring is responsible for a portion of medullary thyroid tumours. Mutations in the RET gene have been linked to multiple endocrine neoplasia, type 2, and familial medullary thyroid cancer. Thyroid cancer risk is increased by familial medullary thyroid carcinoma. The risk of thyroid, adrenal gland, and other malignancies is elevated by multiple endocrine neoplasia, type 2.
Other rare types.Thyroid cancer is also the site of other extremely rare forms of cancer. The immune system cells of the thyroid are the starting point for thyroid lymphoma, while the connective tissue cells of the thyroid are the starting point for thyroid sarcoma.
Risk factors
Thyroid cancer risk factors that could rise include:
Female sex. Compared to men, women are more likely to develop thyroid cancer. Experts believe that oestrogen may have a connection to it. Individuals allocated to the female sex at birth typically have greater body oestrogen levels.
Exposure to high levels of radiation. Thyroid cancer risk is increased by head and neck radiation therapy treatments.
Certain inherited genetic syndromes. Familial medullary thyroid cancer, multiple endocrine neoplasia, Cowden syndrome, and familial adenomatous polyposis are among the genetic syndromes that raise the risk of thyroid cancer. Thyroid cancers that might occasionally run in families include papillary and medullary thyroid cancers.
Complications
Thyroid cancer that comes back
Despite effective treatment, thyroid cancer can recur, and it can even do so after thyroid removal. If cancer cells proliferate outside of the thyroid before it is removed, this might occur.
The majority of thyroid malignancies, including the two most prevalent varieties, follicular and papillary, are not expected to return. Depending on the specifics of your case, your doctor can advise you on whether there is a higher chance of your cancer coming back.
If your cancer is aggressive or spreads outside of your thyroid, recurrence is more likely. Recurrences of thyroid carcinoma are typically discovered during the first five years following the first diagnosis.
The prognosis for thyroid cancer that recurs is still favourable. Most patients will receive successful treatment, and it is frequently curable.
Thyroid cancer may recur in:
(1) Lymph nodes in the neck
(2) Other areas of the body, such as the lungs and bones
(3) Small pieces of thyroid tissue left behind during surgery
For the purpose of looking for indications that your cancer has returned, your doctor can advise routine thyroid scans or blood tests. During these consultations, your physician might enquire about any indications or symptoms of a thyroid cancer recurrence, such as:
(1) Neck pain
(2) A lump in the neck
(3) Trouble swallowing
(4) Voice changes, such as hoarseness
Carcinoma of the thyroid that spreads (metastasises)
There are situations when thyroid cancer spreads to adjacent lymph nodes or other body parts. It’s possible that the cancer cells that spread will be discovered at your initial diagnosis or after therapy. Most thyroid tumours do not spread in the long run.
Thyroid carcinoma typically spreads to the following places:
(1) Skin
(2) Liver
(3) Brain
(4) Lungs
(5) Bones
(6) Lymph nodes in the neck
When you are initially diagnosed with thyroid cancer, imaging tests like CT and MRI may reveal thyroid cancer that spreads. Your doctor may advise follow-up sessions to check for any indications that your thyroid cancer has spread after a successful course of therapy. Nuclear imaging scans, which employ a radioactive form of iodine and a specialised camera to detect thyroid cancer cells, may be part of these consultations.
Prevention
For those with an average risk of thyroid cancer, there is no known source of the gene mutations that result in the majority of cases; therefore, there is no treatment to avoid thyroid cancer.
Prevention for people with a high risk
Prophylactic thyroidectomy is a thyroid operation that may be considered for adults and children who have a hereditary gene that raises the risk of medullary thyroid cancer in order to prevent the malignancy. Speak with a genetic counsellor about your options; they can discuss your treatment options and thyroid cancer risk.
Prevention for people near nuclear power plants
People who live close to nuclear power facilities in the United States may occasionally receive medication that prevents the thyroid from being affected by radiation. If a nuclear reactor disaster were to occur—which is quite unlikely—the drug potassium iodide may be utilised. For additional information about safety procedures to take if you live within 10 miles of a nuclear power station, get in touch with your state’s or your local emergency management department.